This is major news when it comes to genetic breakthroughs and personalized medicine.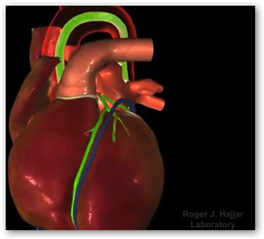 The product is still actively in a clinical trial and has 250 patients enrolled. This is considered a “breakthrough” technology at the FDA. The process has a target using gene therapies to transfer the SERCA2a gene directing into the heart muscle cells and thus there’s a healing effect that takes place allowing the heart to do a better job pumping blood.
The product is still actively in a clinical trial and has 250 patients enrolled. This is considered a “breakthrough” technology at the FDA. The process has a target using gene therapies to transfer the SERCA2a gene directing into the heart muscle cells and thus there’s a healing effect that takes place allowing the heart to do a better job pumping blood.
In trials the treatment helped reduced re-hospitalizations and improved patient quality of life. There were no safety concerns with the treatment. The video below shows how this works and this was a lot of genetic research work.
“MYDICAR treatment involves a one-time outpatient infusion in a cardiac catheterization laboratory, similar to undergoing an angiogram. MYDICAR is designed to restore levels of an enzyme known to play a key role in the progression of heart failure. Repairing this molecular defect in preclinical studies reversed the disease and restored cardiac function. In the Phase 2 CUPID clinical trial in 39 patients, the frequency of death, worsening heart failure, heart failure-related hospitalizations, heart transplant, and need for a mechanical heart pump was dramatically lower and sustained for patients on high-dose MYDICAR compared with placebo. Furthermore, patients’ ability to exercise, symptoms of heart failure and quality of life improved.
MYDICAR’s molecular target is an enzyme found in the sarcoplasmic reticulum (SR) that is critical to the contraction of the cardiac muscle cell. The SR is a specialized part of a cell (cellular organelle) that regulates the contraction and relaxation of cardiac muscle cells by coordinating the outflow (contraction) and inflow (relaxation) of calcium ions (Ca2+). The heart muscle’s ability to contract, and thus to pump blood and maintain oxygenation of the body, is determined by a continual re-loading of the SR with Ca2+ to “stage” for the next cycle of contraction. The key factor that enables the re-loading of the SR with Ca2+ is the enzyme SERCA2a. Numerous human studies have established a clear association between depleted SERCA2a enzyme in cardiac cells and the progression of end-stage heart failure.”
In the first clinical trial patients who had a single infusion treatment had an 88% risk reduction for major cardiovascular events to include death, so this is a good thing. The trials actually separated patients into 2 different groups where one group had higher dosage than the other and both benefited with survival. BD
Celladon Corporation, a clinical-stage biotechnology company developing novel therapies for patients with heart failure and other diseases characterized by SERCA enzyme deficiencies, announced that its lead product candidate, MYDICAR, has been granted breakthrough therapy designation by the US Food and Drug Administration (US FDA) for reducing hospitalizations for heart failure in NYHA class III or IV chronic heart failure patients who are NAb negative.
This designation is intended to expedite the development and review of drugs for serious or life-threatening conditions and where preliminary clinical evidence suggests it provides a substantial improvement over existing therapies.
Celladon is developing MYDICAR as a novel, first-in-class therapy for patients with chronic heart failure due to systolic dysfunction. MYDICAR uses genetic enzyme replacement therapy to correct the deficiency in the enzyme SERCA2a, which is an enzyme that becomes deficient in heart failure patients and results in inadequate pumping of the heart. Celladon has developed a companion diagnostic to identify the patients who are AAV1 NAb negative and therefore eligible for MYDICAR treatment.
Celladon is currently evaluating MYDICAR in the Phase 2b CUPID 2 trial to determine its efficacy in reducing the frequency of and/or delaying heart failure-related hospitalizations. This randomized, double-blind, placebo-controlled, multinational trial is evaluating a single intracoronary infusion of MYDICAR versus placebo added to a maximal, optimized heart failure regimen in patients with NYHA class III or IV symptoms of chronic heart failure due to systolic dysfunction. Patient enrollment has been completed and 250 patients have been randomized in this trial. The company expects to report results in April 2015.





Tidak ada komentar:
Posting Komentar